Years of progress in tackling cancer may have to be written off as a result of setbacks caused by the Covid-19 pandemic, scientists have warned.
More than two years on from the first case, there are early signs that the pandemic may be followed by a rise in the number of serious cancers.
Cancer services were hit hard when the pandemic started in 2020, in common with other parts of the health service. With fear of the new virus outstripping that of cancer, and large parts of the care system off bounds, attendances at treatment centres plunged up to 60 per cent before recovering.
Repeated waves of the virus turned an initial blip into a longer-lasting problem, the full extent of which has yet to be assessed.
READ MORE
The initial problems caused people to miss tests and appointments, and suffer delays in their treatment. Experts say this is now translating into cancers being diagnosed at a later stage, resulting in poorer outcomes for patients.
Doctors are now in a “race against time” to identify cases, so they can be treated as early as possible, according to Prof Mark Lawler, professor of digital health at Queen’s University’s Belfast’s medical faculty.
“Those missed diagnoses from earlier in the pandemic, the people with potential cancers, are still out there. We’re starting to see some of them present later with more aggressive disease.
‘I’m really worried about bed capacity and resources. We are so short on nurses. Staff are burnt out and exhausted from managing high ratios of patients on the wards’
“If we don’t act now, we get the scenario where the Covid-19 pandemic leads to a future cancer epidemic. Obviously, none of us want that.”
“We have a big problem,” says oncologist Prof Janice Walshe. “In the pandemic, people were definitely ignoring worrying physical signs due to concern over Covid. Now, with the perception that everything is gung-ho again, patients are worried that they neglected those signs before. So they want things evaluated and they’re impatient when they can’t have the answers tomorrow.”
“Some element of stage shift is expected, meaning it is likely that there will be a greater proportion of people diagnosed with a cancer at a more advanced stage,” explains Dr Triona McCarthy, public health consultant at the National Cancer Control Programme. “This is also the expectation internationally, but we don’t know this for certain yet.
“For the patient, that could mean the difference between a stage one cancer being treated by surgery alone, and having to also get chemotherapy or other complex treatments if they have a later stage cancer. There could also be an effect on patient outcomes.”
Walshe notes that patients are being diagnosed later and are more likely to have symptoms. St Vincent’s University Hospital, where she works, normally diagnoses about 700 breast cancer cases a year. This figure dipped to fewer than 600 in the first year of the pandemic, but rose to 850 last year.
Services are struggling to play catch-up when resources are limited and staff are suffering burnout. “I’m really worried about bed capacity and resources. We are so short on nurses. Staff are burnt out and exhausted from managing high ratios of patients on the wards,” Walshe says. “Our nurses are going abroad for better conditions and pay, to places where it is easier to get accommodation. And if people aren’t leaving the country altogether, they’re leaving the capital.”
McCarthy says the biggest problem the cancer programme faced in later pandemic waves was staffing. “Even though money had been poured into additional hours for clinics to increase capacity, we were really treading water because of staff absences due to Covid.”
Walshe is concerned that so many cancer patients get caught up in emergency departments, and have to wait hours for admission in risky, overcrowded environments.

One comfort is that breast cancer is less likely than other cancers to spread aggressively before it is detected through the BreastCheck screening programme. Walshe says it is too early to know if the long delays in screening caused by the pandemic will translate into more cancers and mortality.
According to Lawler, doctors in many countries are already seeing excess deaths among their cancer patients, especially in those with cardiovascular and other conditions.
Survival rates for the main cancers have been improving in recent years, but he says “we could lose all of that impact, all we’ve done in a decade, based on what happened in a year. Certainly for colorectal cancer, we may have set ourselves back a decade in terms of five-year projected survival”.
“We’re now starting to see increases in cancer deaths, rather than based on our projections or modelling. It will take another couple of years to say how much, but we are starting to see a difference.”
“We have to realise the pandemic had profound psychological impacts on people with cancer, and not just physical ones,” says Rachel Morrogh, advocacy manager at the Irish Cancer Society.
Due to Covid restrictions, some patients receiving a cancer diagnosis had the news delivered to them while dressed in full personal protective equipment with no family present, she says.
“There was heightened anxiety, as vulnerable people worried about catching Covid, along with the emotional consequences of self-isolating. Some, such as those with blood cancer, still have to isolate.”
And while services were to some extent protected and prioritised by Government, it proved difficult to continue them when so many healthcare workers were falling ill or being diagnosed as close contacts.
Lawler was first alerted to the threat posed to cancer care early in the pandemic when colleagues remarked that people were more afraid of Covid than cancer.
A quick study confirmed his fears: a few months into the pandemic, seven out of 10 cancer patients in the UK weren’t going to the GP or were being referred; and just four out of 10 were getting their chemo on time.
‘Getting better data needs to be a cornerstone of cancer care in Ireland. During the pandemic, we found that the data wasn’t as strong as we would have liked’
He alerted the European authorities to the scale of the problem. Experts sat down with patients and patient advocates to draw up a plan for action and commission a data study across the continent.
“What we saw was pretty shocking. One hundred million cancer screening tests missed, one million people with undiagnosed cancer and a significant backlog in services,” says Lawler. “Meanwhile, three out of every 10 cancer healthcare professionals were showing signs of burnout and four out of 10 had signs of depression.”
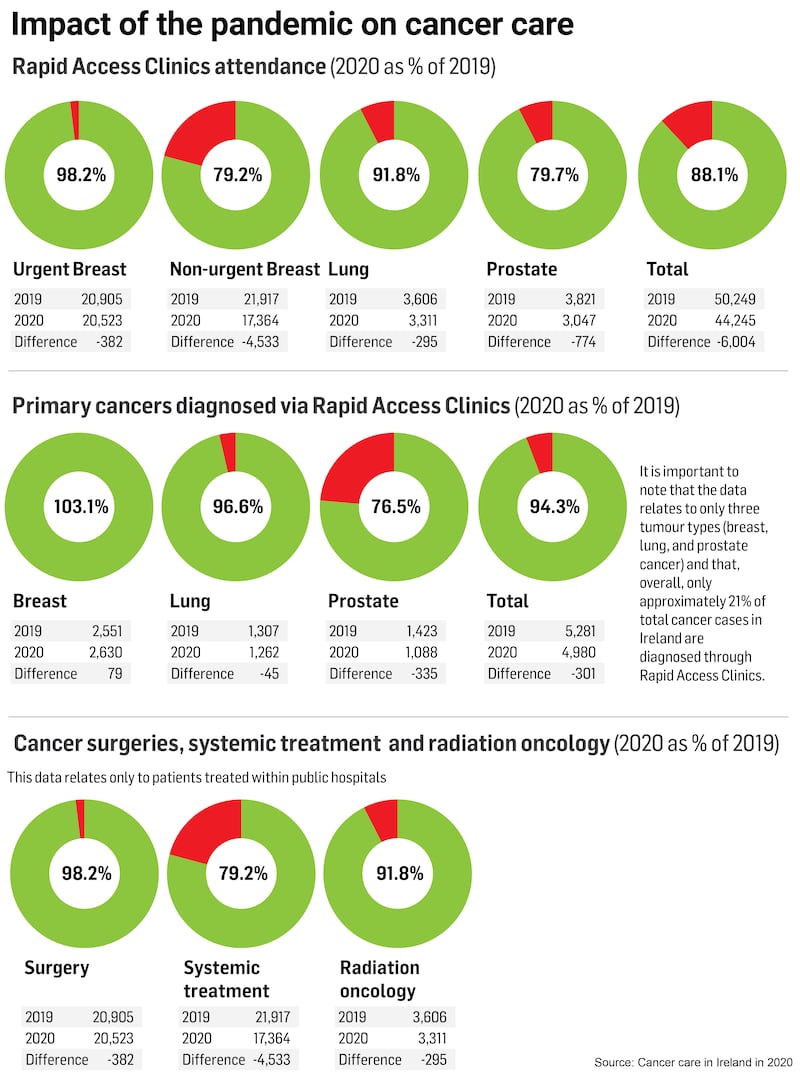
In 2020, the number of cancer diagnoses dropped 10-14 per cent, according to a report published by the Royal College of Physicians of Ireland (RCPI) last December. As for surgery, resections in 2020 were at 96 per cent of 2019 levels – equivalent to 740 fewer procedures.
The impact of delayed presentations and disruptions to diagnoses and treatment on patient outcomes is “not yet quantifiable”, the report found. “Delays in diagnosis of cancer can lead to cancer being diagnosed at a later stage of the disease, when treatment options are limited, and prognosis is poor.”
Lawler rates Ireland’s performance in maintaining cancer services during the pandemic as “probably in the middle” in European terms. The lack of electronic patient records in Ireland’s health service has hindered a proper assessment of the situation. In a fast-moving situation, scientists need to be able to access data quickly so they can spot the most recent trends. “It’s no use having data that’s six months or 12 months old, you need data that’s weeks old rather than months and years old,” Lawler says.
“Getting better data needs to be a cornerstone of cancer care in Ireland,” says Murrogh. “During the pandemic, we found that the data wasn’t as strong as we would have liked.”
In Ireland, the cancer programme is a crown jewel in the health service. Across Europe, cancer services are generally far better developed than for other major killer conditions.
Yet the pandemic showed that cancer services “weren’t as good as we thought they were. It was an unprecedented insult to the system and it shows we weren’t as well prepared as we ought to have been, especially in relation to early diagnosis,” Lawler argues.
Despite the lingering problems, the pandemic delivered lots of positives, Walshe believes. “We modified our practice so we don’t have huge hordes of people sitting on seats in hospital who don’t need to be there. If they are doing well, they can get help perfectly well over the phone.”
When Walshe holds a clinic, half of it will be virtual, and half face to face. “I generally see people face to face when they are new, or they can’t tolerate the medication or I have to give them bad news.”
‘The fact that Covid shone a light on what needed to be improved in cancer services, and what changes could be made with increased investment, was no harm’
“But you can’t rely on telemedicine 100 per cent – sometimes you have to look into the whites of the patients’ eyes.”
McCarthy says initiatives were fast-tracked due to the threat posed by the virus. For example, the creation of an acute oncology service staff by skilled oncology nurses had been in the cancer strategy but only became a reality during the pandemic. In addition, 26 new advanced nurse practitioner roles were approved for centres across the country.
“Another example is the introduction of a new treatment known as SABR (stereotactic ablative body radiotherapy). This new technique allows very focused doses of radiation to be delivered in high doses, meaning fewer radiotherapy sessions for patients.”
The pandemic also saw GPs given greater scope to order scans for their patients.
“The fact that Covid shone a light on what needed to be improved in cancer services, and what changes could be made with increased investment, was no harm,” McCarthy says.
The National Cancer Registry is working on updating its figures for 2020 and completing a preliminary assessment of 2021 data so that a more comprehensive picture of the impact of the Covid pandemic on cancer care can be arrived at.


















