Annie Curbelo Lang recently rented a house in Boyle, Co Roscommon, after spending most of the pandemic staying with a friend. At 69 she still works in a job organising work placements for third-level students and enjoys it. Despite a brush with skin cancer she is in good health generally and has had both hips replaced. But lately she has been thinking about where she might live as she ages.
“I don’t want to go to a residential home when I get older. The idea abhors me,” she says.

From Dublin originally, Curbelo Lang worked abroad for many years in a variety of jobs before returning to Ireland. In Italy she ran her own language school. In Spain she was a riding instructor. She lived also in Australia and Britain. A nursing home is not for her, she believes. “The idea of sitting there with a load of other older people and not doing very much does not exactly make me feel it’s a great ending to my life,” says Curbelo Lang, who has one adult daughter.
“If I’m completely incapacitated I can’t do anything, that’s another story. While I still have my brain about me I want to be contributing to the world that I live in, myself as a person. To be able to do that you need to be able to love the place where you live, to be happy about your surroundings. So I would not be happy in a residential home.”
Curbelo Lang likes the notion of living in a retirement complex, somewhere with private accommodation and access to communal areas. But she doesn’t know of any in her area and wonders what it would all cost. “No matter how much you like someone you still need to have your own space that you can go off to and not be disturbed by people – and then to have a place where you can all get together to enjoy a meal together or coffee. But equally so to be independent in your own space.”
In an ageing country that will undergo a profound demographic shift in coming decades these are questions that will be asked again and again as people live longer. Although the Irish are still young by European standards, there will soon be substantially more older people.
The eldercare system was already creaking before the onset of Covid-19 exposed serious deficiencies in nursing-home care, raising questions about the treatment of some of our most vulnerable people. Ensuring that system is fit for purpose in the future will be a key challenge for society as Ireland emerges from a pandemic that still poses a grave threat to public health.
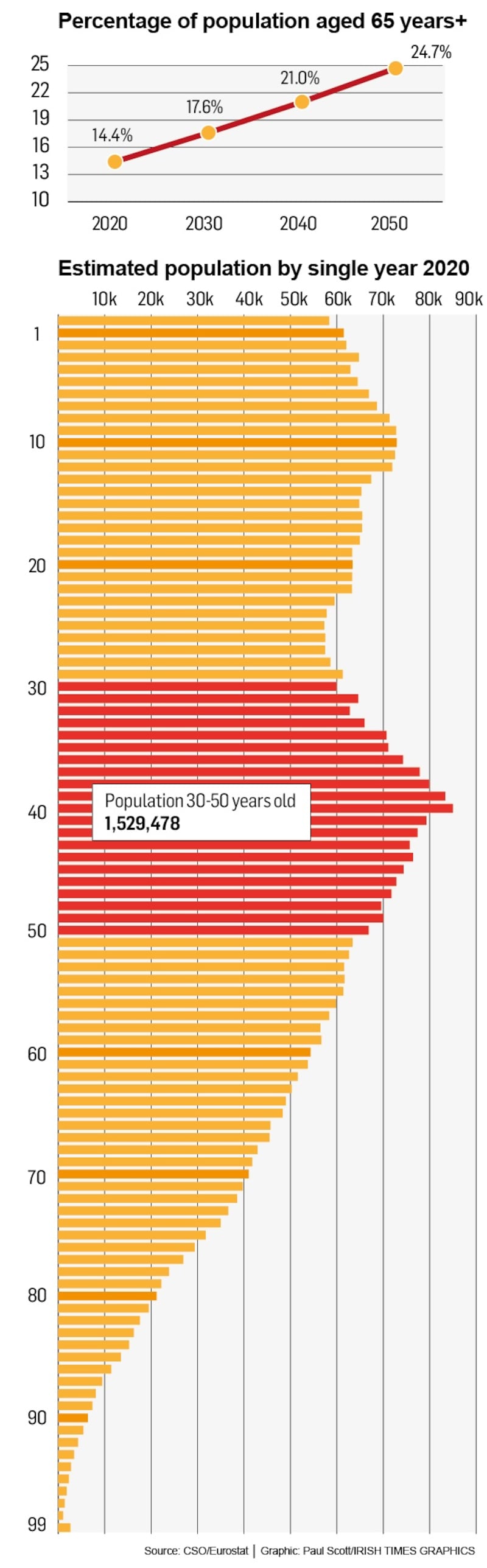
There is no avoiding the ticking demographic clock – and the numbers are stark. In the 2016 census Ireland had 630,000 people aged 65 and over, just above 13 per cent of the population. "That figure is projected to rise to about 1 million by 2031 and to about 1.6 million by 2051," says James Hegarty, a statistician with the Central Statistics Office.
Looking after the needs of these people is shaping up to be a defining test for the State
“The projected increase in the older age population is primarily down to ageing. In terms of the bulk of our population, there are currently just under 1.5 million persons in the 30 to 50 age group. Over the next 35 years, they’ll steadily age to become 65 and over. At the moment we have about 50,000 people becoming aged over 65 every year. Over the next 15 years, this number is projected to build steadily to around 70,000 per annum as the population ages by 2035.”
There is more: “The number of persons aged 80 and over is projected to rise from 148,000 in 2016 to between 536,000 and 549,000 in 2051. That’s an increase in that group of between 260 and 270 per cent.”
Such changes are no different to what is happening in developed countries around the world, albeit a little later in Ireland’s case than countries with older populations like Germany and Italy. But looking after the needs of these people is shaping up to be a defining test for the State.
The thrust of public policy into the future will be to provide more care for older people in their own home for as long as possible – the homecare option. This has been cast as the best way forward for decades but has proved exceedingly difficult to achieve in Ireland.
"All the evidence is that people want to remain in their own homes," says Eamon O'Shea, economics professor at NUI Galway, a specialist on ageing issues and also a former Tipperary hurling manager.
“We’ve had a policy which is good on rhetoric and not so good in terms of delivering on the pursuit of homecare that we all aspire to. When we did try to initiate policy change … we tended to focus on residential care,” he says.
“We tended to neglect homecare. Now that has changed in the last number of years a little bit as we have I think begun to shape a clearer understanding of what’s required in regard to homecare.”
But there is a mountain to climb. “Ireland is slightly below the OECD average [spend on long term care] of 1.5 per cent of GDP, well above southern and central European countries but well below Nordic countries and Japan,” says Ana Llena-Nozal, an economist with the Organisation for Economic Cooperation and Development (OECD).
The European Commission recently highlighted the State's "over-reliance" on informal care, and warned that the adoption of new formal schemes as people grow older will be very expensive.
Government spending on long-term care was 1.3 per cent of gross domestic product in 2019, and is forecast to rise to 1.6 per cent of GDP by 2030 and 2.4 per cent by 2050. According to the commission, a 2050 “risk scenario” could see spending reach 3.2 per cent of GDP.
“These rises are very significant, especially those for the longer term (implying a nearly trebling of the 2019 expenditure levels), indicating significant costs involved for Ireland in relation to a shift between informal and formal care and further development of the [long-term care] system,” it said in a July report.
“Ireland has significant under-provision of public services for [long-term care] and therefore high unmet need. The homecare sector in particular has not kept up with demand, and Ireland is still trying to undo the effects of the cutbacks that were made as a response to the 2008 recession.”
Celine Clarke, head of advocacy for Age Action Ireland, which campaigns for the rights of older people, says the current homecare services are underfunded and undersupplied. “Pre-pandemic figures show over 7,000 people on the wait-list for homecare supports.”
In the programme for government last year, the Fianna Fáil-Fine Gael-Green Coalition promised a statutory homecare scheme. The lack of such a scheme means there is no regulation on the provision of homecare services or indeed on the quality of homecare. A spokeswoman for Mary Butler, Minister of State for Older People, said work is “ongoing” on a statutory scheme with a pilot programme to reform the service due to start later this year.
Colette Kelleher, a former independent senator who was chief of the Alzheimer Society of Ireland, says a statutory scheme ranks among the most important steps for the future. “That’s been talked about for a very long time. It was postponed and postponed,” she says.
In a statutory regime the service would expand. It would also subject providers to independent regulation for the first time and become eligible for funding under the Fair Deal scheme, currently limited to nursing homes, in which a portion of the value of a person’s home would be used to pay for their care.
“You would want to make sure that the model you were proposing was the one where the people doing the work were likely to be suitably qualified to do very skilled work in a home environment and also that they would be paid properly to do that work,” says Kelleher.
Huge public spending on nursing homes was still not sufficient to avert the crisis in the sector when the pandemic struck in February 2020
According to Clarke of Age Action Ireland, the current funding model incentivises residential care even though it is much more expensive than homecare. “The disparity in funding levels between the Fair Deal scheme and the total HSE allocation for home supports is self-evident: in 2018 and 2019 the total budgets allocated to the nursing home-support scheme were €962 million and €991.4 million respectively while €412 million was allocated in 2018 and €446 million in 2019 to was directed to home supports.”
Huge public spending on nursing homes was still not sufficient to avert the crisis in the sector when the pandemic struck in February 2020. Data shows that 985 nursing-home residents had died by October, 56 per cent of all deaths in the State by that time. The Oireachtas special committee on the response to Covid-19 said in a report last year that it was “unable to get satisfactory answers” as to why that happened, despite devoting more time to the question than any other. The committee said the number of deaths was “totally disproportionate for a group comprising of 0.65 per cent of the population who were unique in terms of frailty and vulnerability”.
Kelleher, a former senator, notes the lack of laws to protect nursing-home residents “in the way that we have safeguarding legislation for children”. As a result, a social worker who receives a complaint from a resident has no right of entry into a nursing home to investigate. “All of that was very heightened during the pandemic when you had very large numbers of people dying.”
She supports calls for a public inquiry into the nursing home response to Covid-19, as does Clarke of Age Action. Butler’s office said the Government accepts the need for longer-term reform of elder and nursing homecare.
Nursing Homes Ireland, the lobby group for the sector, says smaller operators believe the current financial model has left smaller operators under acute strain. Although large international nursing-home groups have increased their presence in Ireland, 23 homes closed last year. “This is a very significant number,” says NHI. “Smaller nursing homes are informing us they cannot sustain the costs, and a scheme [Fair Deal] that bases fees on geographic and historic pricing, as opposed to legitimate costs incurred.”
That points to inevitability of friction between the Government, whose finances face massive constraints as emergency pandemic spending programmes are wound down, and a sector that provides care for more than 25,000 people. Another 5,000 people live in public nursing homes.
Despite the push for more homecare, thousands of additional nursing-home places will still be needed as the ageing of the population intensifies. Economic & Social Research Institute projections point to the need for 15,600 new places by 2030 above 2015 levels, when there were some 22,340 spaces in private homes.
Prof O’Shea, the NUI Galway academic, says homecare will never replace residential care. “That’s simply not going to happen. The big challenge is to really make sure that we accelerate this shift to ageing in place, which for many people is in their own homes but there are many variations... Before you go into residential care there’s housing with care, for example, where people may have to shift out of their home but not into residential care. There’s also technology which potentially has at least some capability in terms of allowing us to remain in our own homes for longer.”
Back in Boyle, Curbelo Lang says retaining her independence is crucial. “We need to know that there’s a process, that there’s a place where we can feel that we can give our best without being categorised as: ‘You’re an old person, you’re not useful any more.’ It’s not true,” she says. “We’re all going to get old. That’s something for all of us to think about, even when we’re 30.”
Eldercare in Denmark is the envy of many pensioners, not least because much of the service is provided free of charge.
“Since the tax that you pay in Denmark is quite high, people will also expect that when you get older you will then benefit from all the tax that you paid during your working life, so naturally the state will take care of you,” says Katrine Vedel, chief adviser with Health Care Denmark.
Although people in residential homes must pay rent and utilities, there is no fee for most of the services they receive. “[Long-term care] is organised by 98 municipalities, delivered by public and private providers, mainly free of charge and financed through general taxation,” said a recent European Commission report.
“The system is among one of the most universal and comprehensive in the world. It covers everybody in need of care irrespective of age, income, assets and family.”
Denmark has invested heavily over decades in such services. The country is older than Ireland, with 19.9 per cent of the population aged 65 and more in 2020 compared to 14.4 per cent of the Irish population. But its spending on long-term care is far greater still. The Danes spent 3.5 per cent of gross domestic product on long-term care in 2019. Ireland spent 1.3 per cent.
Large institutions with multiple beds in each room like a hospital ward were phased out more than 30 years ago
There are five types of special housing for older people: nursing homes are institutions with permanent staff and service areas; sheltered housing is linked to such institutions, some with staff and service areas; older-people housing provides homes with staff and service areas; general older-people homes have no staff or service areas; and private-care accommodation consists of homes for people with extensive needs for services and care.
But these rank among the latter options in a system that has gone to great lengths to help older people stay in their own home until they have no other realistic choice. “Homecare covers personal care, practical help and support, and food services. Personal care consists of help in maintaining personal hygiene, to get dressed, to get out of bed, and to eat. Practical help and support covers cleaning, laundering and shopping,” the commission said.
There is a ban in Denmark on building traditional old-age and nursing institutions. Large institutions with multiple beds in each room like a hospital ward were phased out more than 30 years ago.
“We tend to have the principle for a very long time since the 1980s of people staying for as long as possible in their own home, which means that the average age of admittance into an eldercare facility is much higher in Denmark than it is in other countries,” says Vedel.
“We’ve been using a lot of technology in the home in order to facilitate a longer stay,” she adds.
“We have a lot of solutions to support lifting and turning. They are less physically demanding on the carer. That means that there isn’t that much stress on the carer. That means some tasks that would have previously required two carers can be carried out by one.”

















