Michael Hughes cared for his partner Christine at home in Artane, Dublin for years before her deterioration from Alzheimer’s forced him to seek a place in a nursing home for her.
“She was at home with me for six years and I did everything they did in a nursing home,but she was mobile at that stage. It was when she couldn’t walk that it became a serious difficulty for me. I had home help coming in to me but I couldn’t rely on them,” he says.
“When she was mobile, I brought her everywhere and anywhere, but then with Alzheimer’s, it can change quickly. She started to drop cups, and not know how to hold a fork. In the space of a month, she had gone from me bringing her out and about to her being in a wheelchair.”
The coronavirus pandemic has changed everything for Hughes.
He has not visited his wife at her care home, Tara Winthrop in Swords, north Co Dublin, since nursing homes closed to visitors in March.

Hughes sees no point in visiting now as he can sit only in a designated area, a physical distance of two metres away from her and behind a see-through screen – all visiting conditions designed to meet HSE and public health requirements to protect residents against the virus during the pandemic, the home says.
Christine is chair-bound and unable to speak so he feels a visit under these conditions would be futile.
“If I am not up close to her, she would not see me. It would only be upsetting for me to have to go up and see her,” Hughes says, unhappy with the Covid-19 visiting arrangements.
He feels he has been “closed out” from caring for his partner of 20 years and wishes he could don a mask, gloves and other protective equipment in order to get close to her again after her own recovery from catching Covid-19 in the nursing home. The nursing home says that it does not allow visitor access to any other areas as part of its strict controls to protect the residents and staff from the virus.
“She knew my voice prior to lockdown and I’m not sure if that is still the case,” he says.
Stay at home
The worst public health crisis in a century is forcing a variety of rethinks across a variety of sectors of our society, and none more so than in the care of the nation’s elderly population, the people most affected by the virus.
The disease has cost the lives of 991 nursing home residents, or 56 per cent of the 1,763 deaths from the virus in the State. Clusters of infection have been found in 267 residences, or 46 per cent of the country’s 577 nursing homes. Nursing home residents account for one in every five of the 25,826 known cases of the disease.
No sector of society could endure such an emergency without it leading to a serious reassessment of how older people are cared for in congregated settings that leave them more vulnerable to infection and at a higher risk of death.
Leo Varadkar, as taoiseach, was one of the first to reflect publicly on the planned model of elderly care into the future. During an appearance on The Late Late Show in May, he questioned the established wisdom of building lots of modern, high-quality 150-bed nursing homes with single rooms in light of the experience so tragically learned from the pandemic.
“Maybe we need to enable people to stay at home for much longer if possible,” he said when asked whether he had any regrets about his handling of the epidemic.
The crisis has exposed an absence of alternatives to nursing home care and the need for changes to elderly care. The risk of a second wave injects an urgency into the exercise.
“This is as big a wake-up call for how we care for our elderly and vulnerable people as 2008 was to how we regulate the banks,” says Joseph Musgrave, chief executive of Home and Community Care Ireland, whose members employ 10,000 carers who support 20,000 people at home.
There are about 30,000 people living in nursing homes, or roughly 4 per cent of the country’s over-65s population. The gap between home care and nursing home care is seen as a place where alternatives should be found, with new, staggered models of care between the two as well as wider-society solutions such as new types of housing suited for older people.
Everyone wants to stay home as long as they can but home is not the right place for a lot of older people
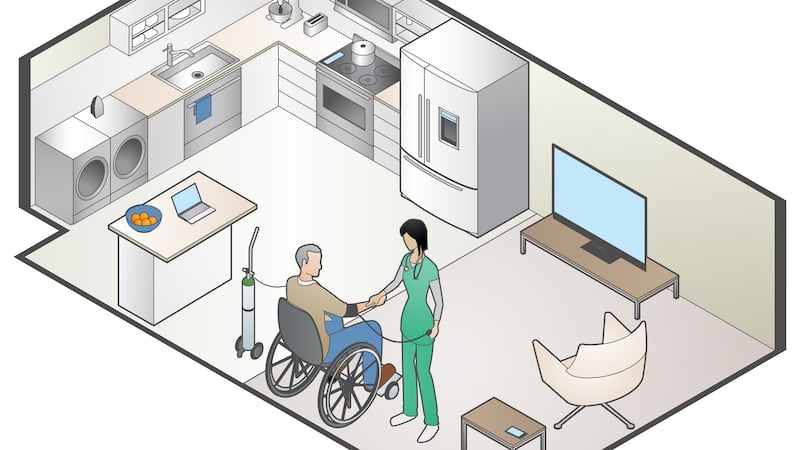
Home care is seen as an attractive solution in the midst of this pandemic as it keeps vulnerable, older people out of higher-risk, congregated settings such as nursing homes.
Musgrave says Covid-19 cases peaked at just 91 out of 20,000 people who were being cared for at home, while there were 7,455 cases across 468 clusters in all residential care facilities.
“Vulnerable people are far safer cared for at home,” he says.
More sophisticated model
The HSE recently agreed in a meeting with Musgrave to pay for 4,000 more home care packages at an estimated annual cost of €50 million to help free up capacity in the hospitals for a potential second wave of coronavirus infections.
Nursing home operators, however, argue that home care does not suit everyone.
“Everyone wants to stay home as long as they can but your difficulty is that home is not the right place for a lot of older people,” says Tim Murphy, chairman of Brookhaven, a group with five nursing homes that managed to limit the impact of Covid-19 to a single death.
“You are delighted to have residents who can get the two to three hours of care a day, but what happens when the carer is gone? They are still susceptible to falls and if you are talking 24/7 care, you are talking three shifts of carers and someone needs to stay over, which raises other issues.”
The nursing home and home care sectors are in agreement that solutions lie in what they call a “continuum of care”.
“The debate for me is community care versus acute care,” says Tadhg Daly, chief executive of Nursing Homes Ireland, which represents private nursing home operators that make up 80 per cent of the sector.
“We need a much more sophisticated model of community care; that means day care, meals on wheels, independent living, home care and enhanced home care.”
Musgrave also sees new opportunities beyond the “black and white” either-or between basic care at home and all the care an older person could need in hospital.
“There is more than just home care here. There is a different design philosophy we need for houses. There is a different philosophy we need to take with technological innovation and healthcare,” he says.
Technology
The shift to virtual health during the pandemic, as doctors kept sick and medically vulnerable people Covid-free and away from hospitals, shows the role that technology can play in freeing up resources and capacity in hospitals while caring for people at home.
Murphy sees major capacity challenges in hospitals and nursing homes as smaller care homes will be forced to close because they are unable to meet the demands of the pandemic, and the HSE comes under increasing pressure to reduce multi-occupancy rooms in public nursing homes without ministerial derogations from increased single-room occupancy quotas.
“I see limited change. It is really challenging to try to put in a new model into the system and build new facilities in the current climate with the lack of capacity in hospitals and nursing homes and a very challenging budgetary deficit for the Government post-pandemic,” he says.
With that in mind, the “who is going to pay for it?” question rears its head regularly in the debate on how care for the elderly can be changed in the wake of this health crisis.
The State’s Nursing Homes Support Scheme, better known as Fair Deal, which subsidises the sector by topping up residents’ contributions from income, assets and savings to cover nursing home fees, has its problems. Private nursing homes regularly bemoan the 60 per cent premium the HSE-run nursing homes receive: weekly payments of €1,665 per week for providing care to nursing home residents compared with just over €1,000 a week paid on average to private homes through the State’s National Treatment Purchase Fund.
Tim Murphy says that the one-size-fits-all approach to the various types of care within the nursing home sector – acute, palliative, dementia and general – works because it has to.
“We are forced to make it work, but society’s and the Government’s big problem is, how do you fund that care if you take part of it away and have to fund different settings?” he says.
People don't do well in large, congregated settings. They become very institutionalised
He argues that bringing dementia care in nursing homes up to a European standard would require either more money to build better homes or smaller homes with more State subsidies.
“Unless you double the weekly cost of dementia care for patients, you cannot do it. It just doesn’t make sense,” he says.
This will become a more pressing issue for the long-term care sector as the complexity of care within nursing homes is increasing with more than 50 per cent of nursing home residents having dementia or some form of cognitive impairment.
‘Incentivising institutional care’
Paddy Connolly, chief executive of Age Action, the advocacy group for older people, says that Fair Deal “incentivises institutionalised care” as nursing home care is viewed through an investor’s lens of value for money, leading to larger and larger homes and commodifying care.
“People don’t do well in large, congregated settings. They become very institutionalised, it becomes about staff rotas and treating people as groups where there are only two things on the menu and residents are all directed to ‘go over there and told to do this and do that’,” he says.
One alternative is to create an integrated system for long-term care, covering both home care and nursing home care, where money would be assigned based on a person’s care needs. This could determine – and cover the cost of – caring for those who can remain at home and those whose needs are so great that they require 24/7 support and nursing home care.
Joseph Musgrave likes the German system, where a person’s care needs are assessed and assigned to one of four care grades and they receive cash or in-kind benefits, depending on what care they need. They then “purchase” services from approved providers in their locality.
Such a scheme could be used to facilitate greater care in the person’s home with family members receiving pay for caring for relatives in order to keep them at home longer.
"We are going to need to make better use of all money that we have, to keep more people out of more serious forms of care so we can make the resources work better," says Mervyn Taylor, director of Sage Advocacy, a group that represents vulnerable adults.
Age-friendly housing
Varadkar’s idea of keeping people at home for longer may require more radical solutions beyond the type of care they receive. It will require building new types of housing – well, new for Ireland – for a much larger, ageing population over the coming decades.
The share of the population aged 65 and over is projected to increase from one in eight to one in six by 2030. In the next eight years alone, the over-65s are expected to increase in number by one third and to double over the next 25 years.
The population of people aged 85 and over – the people most likely to need nursing home care – is forecast to more than double over the next 20 years.
That means a lot more older people to find the right homes and right long-term care for, whether it is in the community or a residential setting.
A report by Economic and Social Research Institute (ESRI), the State’s independent think tank, published in 2017, projected that demand for long-term care in nursing homes would increase by up to 54 per cent by 2030 (from 2015), while demand for home help hours would rise by up to 66 per cent. Demand for GP visits was projected to increase by up to 27 per cent.
The increased demand for hospital healthcare over the coming decade, with in-patient bed days expected to rise by up to 37 per cent (by 2030 on 2015 figures) due to the ageing population, will likely lead to greater demand for nursing homes to be used as respite and step-down facilities.
At the end of the care spectrum, where people do not require the services of a hospital, there is expected to be major demand for new types of housing for the ageing population.
A Department of Housing report last year estimated that housing requirement for older people by 2031 will be 150,000 units of “rightsizing housing within existing communities – small dwellings designed to meet the needs of older people”, 150,000 units of “age-friendly accommodation” and 36,000 nursing home spaces.
The State needs to take a strong role integrating housing and healthcare policy
This could mean building “retirement villages” similar to those in Australia, New Zealand and the United States, or more apartment complexes catering exclusively for older people, similar to projects such as McAuley Place in Naas and Great Northern Haven in Dundalk.
Ronan Lyons, economist at Trinity College Dublin, says there are shortages of "downsizer" suburban apartments suitable for older people (which could free up much-needed homes for families) as well as independent living and assisted living complexes that could solve the housing needs of an older, ageing population.
“The State needs to take a strong role integrating housing and healthcare policy. It doesn’t necessary need a big policy push, but all those three sectors of housing are actually missing in Ireland,” he says.
Lyons says the Covid-19 pandemic has seeded the belief that older people may be better off staying at home, which may not be the best option for them.
“What Covid has done effectively is solidified the belief people have that ‘well, I am definitely not going to a nursing home until you drag me in there’, because there are other options. But they are stuck in what might that have been their family home from their 30s and they are in their 80s. It may not be an equal fit for their needs,” he says.
The accelerating size of the over-65s age group requires creative thinking and rapid change in providing more options for care and housing with associated care for a greying population.
“The volume of change is just off the charts compared to what we are used to,” says Lyons.
No alternative
For Michael Hughes, the pandemic is keeping his focus not on future sweeping changes across the care sector but on how nursing homes are being managed in this crisis, the visitor restrictions during the pandemic and what it means for his partner and his lack of day-to-day contact with her for four months.
He does not see any options when it comes to the care of his partner other than in a nursing home. “I really don’t see that there is an alternative,” he says.













