An estimated 12,000 people in Ireland are living with Parkinson's disease (PD) and this is projected to rise to up to 20,000 over the next 15-20 years.
However, we don't have adequate data in Ireland, says Prof David Bradley, a neurologist at St James's Hospital in Dublin. These figures are based on extrapolations from studies in other countries.

“It is a condition that is age-related, but I would have a lot of patients where it affects work or even family planning, for example.” It’s “not that unusual” for him to see patients with PD in their 40s and he is quite used to treating ones in their 50s and early 60s.
Yet, it is commonly regarded as a disease of older people, a view still shared even by some clinicians, he suggests. Although, it is being increasingly recognised that those with young onset PD have different challenges, with a lot of interest in unmet needs. It is now accepted that “to win” with such diseases “we really need to understand the patients in front of us and they are not all the same”, he says.
Approximately 60 per cent of people with Parkinson’s are men and 40 per cent are women, but the accuracy of any such statistics are problematic due to the nature of the condition. There is classic Parkinson’s disease and there is also “parkinsonism”, which covers people with Parkinson’s-like symptoms. “They could have Parkinson’s disease or they could have a list of about 40 other conditions or more.”
We're getting closer and closer to the point where you'll have a disease modifying treatment; at the moment we don't have that
It’s certainly feasible, he says, that women with PD could experience hormonal effects on their symptoms. “It is important to know that and to give ‘rescue therapy’, ie higher doses, on demand if needed. The broader picture is that every patient with Parkinson’s behaves differently and there are lots and lots of things that can affect how a patient feels on a given day.”
The menstrual cycle is obviously a factor that men with PD don’t have to worry about “but it is one of many factors, all of which have to be carefully considered when trying to mitigate symptoms”.
Treating symptoms is all that can be done as the search intensifies for a cure. The drug most commonly used in treatment is one developed 50 years ago. “We’re getting closer and closer to the point where you’ll have a disease modifying treatment; at the moment we don’t have that,” says Bradley. “Everything we do, including deep-brain stimulation surgery, all affect the symptoms patients have.”
But successful management of symptoms can be the difference between night and day for patients, he says, and that’s what they aim to do at a weekly specialist, multi-disciplinary PD clinic at St James’s. With early detection, “you can head off complications. You can keep patients well. It’s much harder to recover ground when they become unwell.”
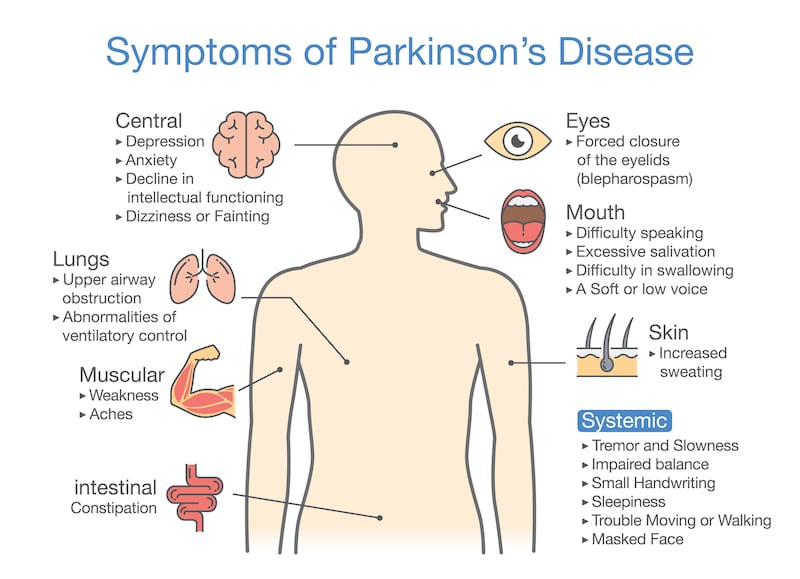
PD shouldn’t affect life expectancy in an average patient if they’re managed well. But they are at risk of complications, for example swallow problems could cause aspiration, which may lead to potentially fatal pneumonia. “The message I usually try and give is that it is a very manageable condition,” says Bradley. Categorisation of PD as a “neurodegenerative” disease may sound very negative, but progression is slow.
Study
However, PD patients do need adequate services for optimal health. The gaps in our healthcare system are likely to be highlighted in a PD mapping study, which is due to be completed next year.
The lack of neurologists is a long-standing problem. The national model of care says there should be 65 for the current population. “At the moment we have 35-40 depending on how you count it.” Some are temporary posts to deal, say, with a particularly long waiting list. It’s not just more neurologists that are needed but all the wraparound services involved in management of symptoms, such as nurse specialists, physios, occupational therapists, speech and language therapists and dietitians.
Not only does the multi-disciplinary structure need to right but there must also be enough resources to deliver for each patient without having to prioritise, he stresses. “That’s an Irish health system gap. If you don’t have the whole team, you can’t get the whole outcome.”
Read: ‘Parkinson’s wants to make your world small . . . ’











