In spite of massive resources poured into research for a cure, cancer continues to frustrate scientists. We now understand that cancer is not one disease but many, and that for example breast cancer and lung cancer should be treated differently. However, it now looks like things are a lot more complicated than that: cancer could indeed be thousands of different diseases. What’s more, cancer could be thousands of different diseases within the same person. Welcome to the cancer ecosystem.
One of the reasons why cancer arises in the first place is damage to the cell which affects its DNA. When a healthy cell divides, it gives its daughter cell an exact copy of its DNA, so that every cell in the family will be the same. Because cancer cells are damaged, they grow faster than healthy cells and don’t carry out all the necessary controls for copying DNA; as a result, cancer daughter cells can be quite different from their mothers. This is known as genomic instability.
"When people think about cancer they see one thing, a sole entity," says Dr Alex Eustace, senior research fellow at the National Institute for Cellular Biotechnology. "People refer to cancer specifically about where it comes from. Historically we have talked about breast cancer or colon cancer, but in reality a lot of cancers can be quite dissimilar to each other regarding their genetic make-up, the way the cancer is wired."
“Inside each cancer there are cells that are going to act in a certain way and cells that will act in other ways. This can have a huge impact on how a cancer develops and how it responds to therapy.”
This is because there are subtle differences in the underlying biology of the tumour
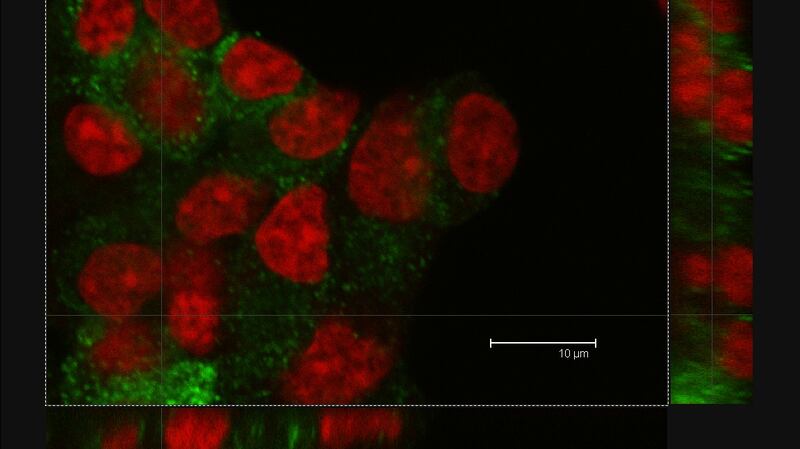
"There are tumours that, if you look at them under the microscope they look very similar, but at the molecular level they can be incredibly different," says Dr Sharon Glynn, lecturer in pathology at National University of Ireland Galway. "Although one person's tumour might look exactly the same, that person's [treatment] requirements would be different from another person's. This is because there are subtle differences in the underlying biology of the tumour from patient to patient and even within the same patient.
“The fact that tumours are so different is probably a combination of different things, such as having inherited certain genes, having particular lifetime exposures like your diet, occupation, even your exercise habits, [although ultimately] we don’t know exactly which combinations are likely to lead to specific tumour types,” says Dr Glynn.
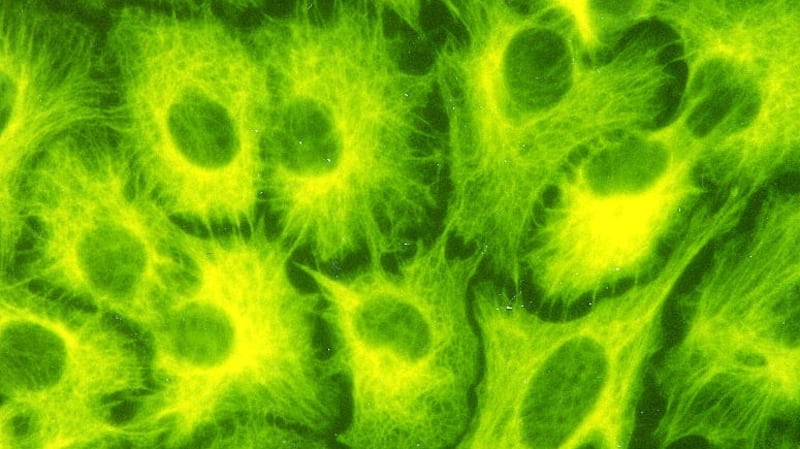
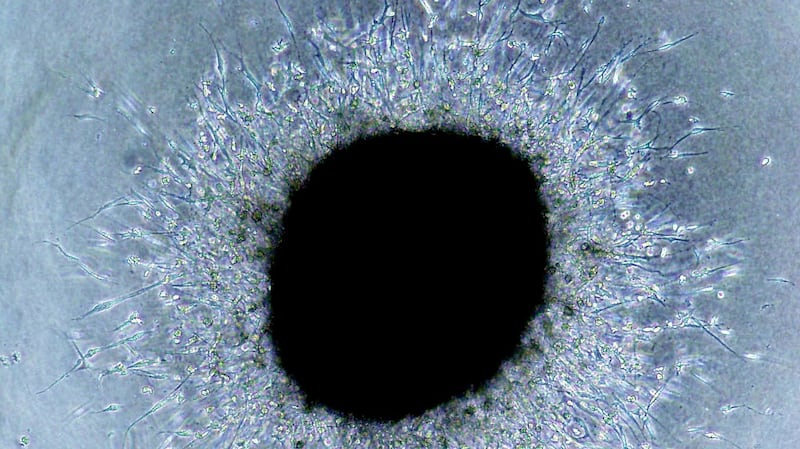
The concept of cancer heterogeneity is not new, but the implications for therapy are becoming more and more apparent. Scientists have been able to take a tumour, separate it into individual cells and label each one with a genetic “barcode”, so that each cell type can be easily identified. They have then implanted the mixture of cells into laboratory animals and followed their evolution.
What they have found is that certain cells are more successful than others and they grow and reproduce faster. All these cells are competing for limited space and resources such as sugar and oxygen and any advantage that a cell has at surviving in this difficult environment results in it growing and reproducing better, taking over and leaving other cells in the dust.
When the tumour runs out of space, some cells might decide to be adventurous and move to greener pastures, spreading to other organs: here they are exposed to completely different circumstances, and only those cells that can adapt to them will prosper.
Sounds familiar? Why yes, this is nothing but Darwinian evolution in action, pure survival of the fittest. Cancer cells are highly variable because of their genetic instability, and then the application of a selective pressure decides which cells come out victorious. These selective pressures can be limited amounts of necessary resources such as sugar or oxygen or, crucially, chemotherapy.
This is usually what happens when a patient first responds to treatment but then relapses
Administering a toxic drug will probably kill most cancer cells, but some may yet survive and, in the absence of competition for food and lodging, grow back to regenerate the tumour with their own kind. This is usually what happens when a patient first responds to treatment but then relapses.
“When you are treating a patient in the metastatic setting, which is generally when heterogeneity is at its greatest, you end up treating what you think of as the primary cancer. This is a successful policy, but problems can arise because you allow smaller subpopulations of cancer cells to redevelop and these cells become the dominant cancer rather than the one you were treating,” says Dr Eustace. “You have a limited window of opportunity to treat that patient and this poses problems for clinicians because in reality they’ll never have enough time to treat each individual cancer which has arisen.”
So what can we do about it? “At the moment oncology scientists are very aware that heterogeneity exists; unfortunately, none of us are in a position to really understand how you can specifically go about treating the cancer when it becomes very heterogeneous in its make-up,” says Dr Eustace.
“We really need to sample the tumour very, very well [as] just one sample might not be representative of the entire tumour,” says Dr Glynn. She goes on to explain that identifying the different cell types present in a tumour could better inform what type of treatment is best for the patient, making it more likely to be successful.
Dr Eustace agrees with this point of view. “By identifying specific subsets of [cells] at least we know what we’re trying to treat at that point. That’s why we want to understand heterogeneity,” he says. He also suggests continued biopsy as a way of monitoring what is happening inside the tumour and what type of cell predominates inside it. “Maybe what we need to do in the future is just keep a better track of cancer,” he says.
Another point Dr Eustace makes is the importance of early diagnosis. Catching cancer early means that it has had less time to develop, and thus has less heterogeneity. “Once the cancer develops you get these different cell populations that coexist inside the same tumour and that makes it much more complicated for therapy to actually work on it.”
We need to be treating with combinations of targeted therapies
It has also become quite obvious that no single drug will be able to control, let alone cure, what is effectively a cumulus of different diseases. “Instead of it being just a single therapy we need to be treating with combinations of targeted therapies in order to target multiple populations of cancer cells at one time,” says Dr Eustace.
Taking into account the parallels between a community of different types of cancer cells within a tumour and an ecosystem, the study of tumour heterogeneity could be further improved by using tools and knowledge generated by evolutionary biologists and ecologists. This might help us drive the cancer ecosystem to extinction.
CAN ECOLOGY HELP?
Oncology experts can talk about cancer being like an ecosystem, but how does it look from the other side? We asked Dr Andrew L Jackson, associate professor of Zoology at TCD.
Dr Jackson’s research aims to understand ecological systems from an evolutionary perspective, focusing on understanding interactions among individual animals living in close proximity. So, can cancer be studied in a similar way?
“I think it’s a very similar process, in many ways,” he says. “[I can think] about cell to cell interactions in the same way as I think about animal to animal interactions.
“Ecology is all about interactions between living organisms, how they can be with each other, how they cooperate with each other sometimes . . . I think cellular systems are in many ways much the same. We have cells that live in close proximity to one another, they have to interact with one another, they might sometimes compete for nutrients. They live in an environment as well, so much like animals live in an ecosystem, the cells live in their own ecosystem, which is surrounded by whatever nutrients are available to them, whatever other cells are out there.”
In many ways, cancer acts as an invasive species
Also like an animal species, cancer cells can change the environment, for example by forcing the growth of new blood vessels in order to feed themselves, Dr Jackson says. In many ways, cancer acts as an invasive species.
“I think a lot of research from cancer biologists, maybe not explicitly but implicitly, considers the host as an ecosystem in which cancer proliferates. And certainly when you think about metastasis, when cancer cells break off from where they were and essentially go seeding or dispersing into another tissue, that is very similar to the process we see in ecology of a species moving and invading new territory. So they are very similar.”
So how can ecology help cancer research? “We’ve got almost 60 years’ worth of really good mathematical theory to understand systems like this. What we would try to do in ecology is to use that theory to make predictions about what will happen in a system, and then go out and test them. If those empirical tests backed up the theory, then we could start using that theory to make predictions for the future, such as if this species moves, gets into this new ecosystem, will it invade or will it not?”
“I think one can see that you could apply something similar to cancer as well, to look at the genotype or the phenotype of the cancer cell and use that to make predictions as to which of these are going to result in either metastasis or which ones are likely to invade or to cause problems more so than others,” Dr Jackson says.
You can't drive a species to extinction without subverting the whole ecosystem
However similar cancer may be to an ecosystem from an evolutionary point of view, it is not exactly the same. And new tools may have to be developed in order to establish the precise differences and generate a useful model oncologists can work from. “We can say that cancer evolves, but the devil is in the detail, and we should work very hard about the specifics of each system,” Dr Jackson says. “Cancer biologists couldn’t just take evolutionary theory and apply it, they have to think carefully about whether the process that’s going on maps well on to it, or to develop new theories that include the understanding about how cancer cells actually spread and are subject to evolutionary process. “
One of the things we know is that you can’t drive a species to extinction without subverting the whole ecosystem, so eliminating cancer could come at a high cost. Are there lessons to be learned from ecology here?
“There are a lot of situations in ecology where we want to drive some species to local extinction. There’s been a lot of cases of rats being introduced [and they] decimate the local bird population who are nesting happily with no predator. And we’ve gone there with the intention of absolutely eradicating the rodents off the island, just completely wipe them out, sometimes with success, sometimes without success. So local extinction in ecology is absolutely a thing that we try to do and it would be similar in a way to the concept of treating cancer.”
Maybe it might be possible to not eradicate the cancer but get it as far under control as possible
“The other thing that we would often do in ecology is try to manage the system, so try to kill or remove a lot of the undesired animals and then manage the system so that we keep their numbers low. So we might supplement or do something to help change the habitat for the native species so that they manage to keep the invasive species at bay, so we basically give the native species a helping hand. I’ve read ideas about that in cancer biology, maybe it might be possible to not eradicate the cancer but get it as far under control as possible, at a regulated level that does not cause pathological problems.”
Indeed, new therapies aimed at stimulating the patient’s immune system to help it fight cancer would be doing just that. So while we can say that lessons from ecology are already being applied to cancer treatment, there is still a long way to figure out exactly how cancer behaves and how we can best treat it.










