On the table at the back of the empty hotel function room, alongside the customary pump-action coffee and tea dispensers and a tray of mini pastries, there is an array of contraceptive devices and testing kits for sexually transmitted infections.
They hint at what is to come.
Up to 150 teenagers from three Dublin schools are heading this way for a morning workshop entitled Debunking the Myths: The Science Behind Our Sexual Health. The free two-hour session is one of a series being run for transition year students by the Royal College of Surgeons in Ireland’s department of obstetrics and gynaecology, in collaboration with the Rotunda Hospital and funded by Science Foundation Ireland. By April, the project hopes to have engaged with 6,000 students from more than 55 schools through in-person and live-streamed events.
At the table of exhibits, which will later be passed through the room, project co-leader Dr Zara Molphy, a research director at RCSI, picks up a flesh-coloured mound encased in clear plastic. It’s a “dummy arm”, she explains, inviting me to press it and feel the contraceptive implant under the surface. These props are all part of helping to make sexual health matters real and tangible for 16-year-olds, who are on the cusp of the legal age of sexual consent, which is 17, but have already passed the age of medical consent, which is set at 16.
READ MORE

The relationships and sexuality education (RSE) curriculum is limited and some teachers are not comfortable delivering it, says Dr Molphy. “They are not experts.” Whereas, at a workshop like this, the students can hear the “raw hard facts” from sexual health experts who are “embedded in the community and aware of all the issues”. This helps to eradicate any stigma, she says, and supplements what is covered in schools.
Unlike their parents, who gleaned information about sex through rudimentary biology lessons and top-shelf magazines, today’s online generation is bombarded with sexual information and imagery. The challenge is discerning what’s true to real life and what’s not.
This is where the “debunking myths” approach comes in. In an era of “fake news”, it can be difficult for teenagers to identify reliable sources of information about sexual and reproductive health.
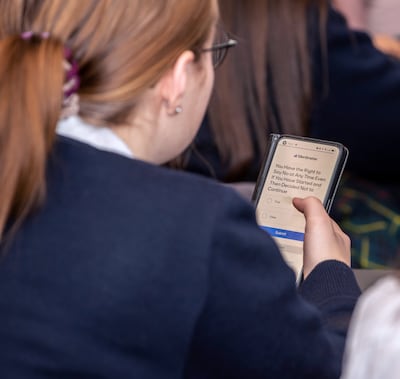
At this workshop they can not only listen to scientifically sound details but are also able to interact anonymously with the speakers through the use of an app. By scanning a QR code with their smartphones, they can use the Mentimeter app to respond to “true or false” polls throughout the workshop and to ask questions. Although, they are told that they can also put up their hands to ask a question if they feel confident enough – nobody does.
Live-streaming these workshops can give them a much wider reach but the project team all agree that the in-person dimension, away from the school premises, is ideal. The teenagers are more comfortable and open, says Dr Molphy, as TY students from King’s Hospital School in Palmerstown, Loreto Abbey Dalkey and Larkin Community College on Champions Avenue, off Cathal Brugha Street, start to file in.
“This is a safe space,” the other co-leader of the project, Prof Fergal Malone, consultant in obstetrics and gynaecology at the Rotunda, says in welcoming participants. The workshop is intended to “empower you to discuss your sexual health comfortably with friends, family and professionals”.

Topics covered during the morning include options for contraception, male and female anatomy, menstruation, sexually transmitted infections, assault and consent. The emphasis is on how to access services for their health needs and what to expect when/if they go there.
While the majority in the room correctly answer the various true or false questions flashed up on screen, it is one about the expense of contraception that catches them out. It seems many are still unaware of the free contraception scheme for women aged 17-26, which was introduced last September, with eligibility extended by a year from January.
Over the two hours, varying levels of hush in the room are probably as good an indicator as any of when the teenagers are learning something new. A session on sexually transmitted diseases, delivered by Dr Kate Jackson from Beaumont Hospital, and another conducted by Dr Dan Kane from the Rotunda’s sexual assault treatment unit, are particularly quietly received.

People aged 15-24 account for half of the 11,000 cases of chlamydia and a third of the 4,000 gonorrhoea infections reported in 2022, according to figures from the Health Protection Surveillance Centre. Samples of the free home test kits available from sh24.ie are explained and passed around, with the assurance that these would arrive through the letter box in a plain envelope with nothing to indicate its contents.
Dr Kane captures his audience’s attention from the outset when he tells them that 24 per cent of people who come into the Rotunda’s sexual assault unit, which sees people from age 14 upwards, are under the age of 18. He also played the Consent – It’s Simple As Tea video, which, if you haven’t seen it, is well worth looking up.
Specific advice on what not to do after an assault and before attending a clinic and what happens when you get there, is information you hope nobody in the room would ever need. But as one question submitted, “If you know somebody who has been sexually assaulted, what can you do for them?”, shows it’s an all too relevant topic for TY students.
Here are three different perspectives on the workshop.
Speaker
“Putting a condom on a banana in front of 200 transition year students probably isn’t everybody’s idea of a fun Friday morning,” says Dr Ronan Daly of the Rotunda’s obstetrics and gynaecology department after leading the opening session on contraception. “But you can see as the session goes on people become more comfortable.” He believes the students come in very keen to learn.
“It’s about giving them as much information about as many different aspects of sexual health as possible. They can be so bombarded with information from so many different places; somebody sitting them down and saying, ‘This is the facts of it; this is based on medicine’, they appreciate and respond to that.”
He believes the workshops come at a critical time for students, who will be going into adulthood imminently. Although the submitted questions will inevitably include many jokey ones, speakers can usually identify three or four that the students have probably never had the opportunity to ask before, he says. “For example, ‘What should I do if I think I have an STI?’ You can tell it’s a genuine concern for one student in the hall and can direct them to the right places.”
Students
Adrian Lucaci (16) from Larkin Community College says he wasn’t expecting the session to be so open about sexual health matters and that such information could be shared without everybody sniggering. He thinks it is good that they could ask questions anonymously through the app because “nobody was going to put their hand up in front of everybody”. He says that he hadn’t known much about sexually transmitted infections beforehand nor how to access various services. Overall, he feels they are better informed now and could share what they had learned with their whole peer group.
Brooklyn Rooney (16), also from Larkin Community College, rates the morning’s workshop as “good and bad”. The good? “The way you get to learn about what girls go through.” The bad? “Just to sit in silence.”
Aimée Halcomb (16) from King’s Hospital School says she found it “really interesting and quite useful for the future. It’s nice to know that Ireland is offering these sorts of things.” She had been unaware, for instance, that the free contraception scheme for young women had started.
Minami Ogura (16) from Japan, who is a boarder at King’s Hospital School, says this country is much more open than her native land. “We can’t talk about this topic,” she says. “It’s embarrassing, not good.”
A fellow boarder, Rebecca Peter (16) from the Black Forest in Germany, reckons attitudes here are similar to those in her homeland, where society is “pretty open”. The workshop has been better than she expected and now she is keen to find out about the corresponding sexual health services in Germany.
Teacher
“Some of this stuff would be new, some of it we would have done before, but what’s fab is taking them out of the school environment,” says Joy Creighton, who teaches “wellbeing”, encompassing the SPHE (social, personal and health education) and RSE programmes at Larkin Community College.
The teachers are careful to stay at the back of the room, out of the eye line of the students, she says, “to give them their space to explore this world”. She was the TY co-ordinator in 2019 when the school did a pilot of this “debunking the myths” programme and the students “loved it”.
This morning she is pleasantly surprised at the level of knowledge, as indicated by the “true or false” polls. “They seem, on the whole, to be quite educated on this.” She also uses the Mentimeter app in classes so her students would be familiar with it.
A workshop like this “is a great support to what we do”, she says, “but there’s another big side to it”. She is concerned about sexual attitudes and behaviour, “the morality of stuff”. She sees the impact of celebrities and influencers, not least Andrew Tate. He seems to be able to “brain wash” young men, adds Creighton, who is about to start studying at Dublin City University for a postgraduate diploma in SPHE and RSE as part of a Government initiative for post-primary teachers.

Myths
The idea that you can only take the “morning after” pill on three occasions in your life and after that it won’t work is one particularly prevalent sexual health myth, according to Dr Daly. The colloquial name for this type of medication also perpetuates the belief that it will only prevent pregnancy if taken within 24 hours of sex, whereas there are options that can be taken for either up to three days or up to five days afterwards.
Other examples of common myths cited by the project include: only girls need to get the HPV vaccine, men and boys don’t need it; the pill protects me from sexually transmitted infections; I can’t get pregnant while I’m on my period; period pain is over-hyped; a circumcised penis is cleaner than an uncircumcised one; teaching sex education makes students more promiscuous.
Dr Molphy debunked some other myths in Health + Family last September.
Tips on keeping safe
Parents tend to have their own repetitive script for teenagers as they disappear through the front door for a night out. You might like to compare yours with words of advice given to students during the session led by Dr Kane.
- [Have your] mobile phone charged and with credit
- Look out for friends, keep together and don’t leave a friend in a vulnerable position
- Trust your gut feeling and act early in uncomfortable situations; be assertive and know your own limits
- Beware of alcohol use, don’t accept drinks from strangers or leave them unattended
- If possible, don’t walk home alone, stick to well-lit areas, get a taxi together
- Tell people where you are going and when you are home safe, for example, use live location/current location on social media apps
- Set up emergency SOS message/emergency contact on your phone















