What is a tick?
A tiny, spider-like, parasite that feeds on the blood of humans, animals and birds. They are more numerous and more active from spring to autumn in Ireland, a time when we are all outdoors more, increasing our chances of encountering them.

Where are they found?
They live in woodlands and damp, grassy undergrowth all over the country, including both urban and rural areas. You could find them in your garden. They like to clamber up a long frond of grass, ideally one that is hanging into a pathway where potential hosts, ie mammals, including humans, will walk along, says Dr Paul McKeown, a consultant in public health medicine with the HSE’s National Health Protection Service.
When a person or animal brushes against them, the tick attaches itself. In the nymph (baby) phase, a tick is only about the size of a poppy seed. But once they have embedded their mouth into the skin and start feeding, they can grow to the size of a petit pois, he explains. If undisturbed, they would fall off once full.

What harm do they do?
The majority of bites from ticks are likely to leave nothing more than a red spot of skin irritation at the site. However, some ticks carry disease and can infect your bloodstream when they latch on.
READ MORE
A variety of tick-borne diseases are mapped worldwide but here in Ireland, Lyme disease is the concern. According to McKeown, it is estimated that only about 5 per cent of ticks here are infected with the bacteria that cause Lyme disease but there is not enough information to be definitive about that.
What is Lyme disease?
It is a bacterial infection. The bacteria Borrelia burgdorferi transfers from a tick’s saliva when it starts feeding on a host’s blood. If Lyme disease is caught early on, appropriate antibiotic treatment is usually successful. But if it evolves undetected or is mistaken for something else, it can develop into a complex, chronic illness. An analysis of pooled data, published in BMJ Global Health in 2022, estimated that 14.5 per cent of the world’s population is likely to have been infected at some point with Lyme disease, as indicated by antibodies in the blood. While acknowledging information gaps, the study also highlighted an increasing prevalence, probably due to climate change.
The disease is named after Lyme, a small coastal town in rural Connecticut in the US where it was first identified just under 50 years ago, in 1975.
Who is at risk?
Anyone of any age who spends time outdoors. This includes ramblers, campers, mountain bikers, people who work or walk in woodland, parkland and heathland, especially in grassy areas. Pets, such as cats and dogs, can acquire ticks, which could then attach on to a human. This is more likely to happen if pets frequent their owners’ sofas or beds. (You can read more about tick infections of pets on the website of the European Scientific Counsel Companion Animal Parasites, esccap.org.)
Obviously, the longer you are out in areas of denser tick populations – counties Galway, Kerry and Wicklow have been identified in past studies as among Ireland’s hotspots – the greater the risk. If you are holidaying abroad, you should know there is a much higher incidence of Lyme disease in many parts of the United States and also in other areas of Europe. The European Centre for Disease Prevention and Control (ecdc.europa.eu/) maps the current known distribution within Europe of the tick species Ixodes ricinus, which carries Lyme disease.
How can we prevent tick bites?
- Staying on paths in woods and grasslands, to try to avoid close encounters with ticks, is a good start.
- Wear long trousers, long-sleeved top and shoes.
- Put on a hat and tuck in hair.
- Use an insect repellent (preferably containing DEET) on clothes and any exposed skin. If you’re worried about which one is safest to use on a child, ask your pharmacist for advice.
- It is a good idea to wear light-coloured clothing so ticks are easier to spot and brush off before they get anywhere near skin.
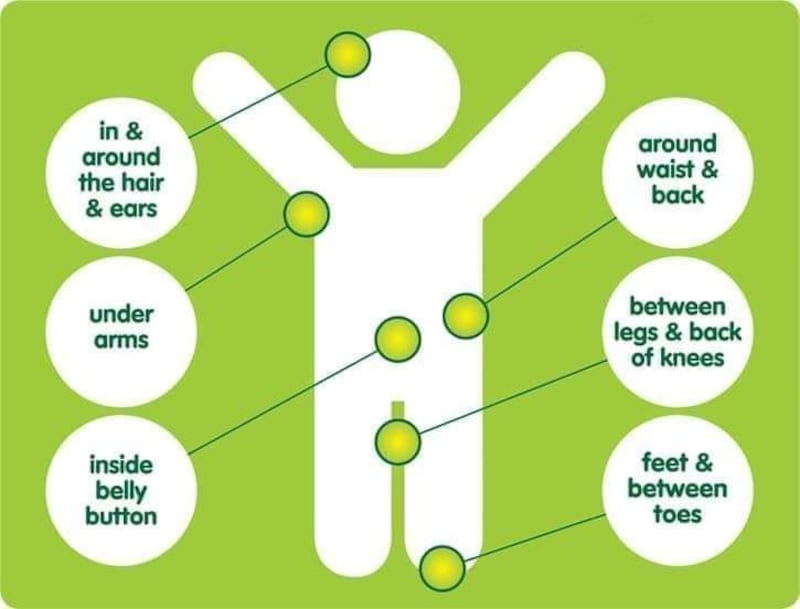
- During a day out, or certainly on your return, check skin, hair and warm skin folds for ticks. In children, the bites are most likely to occur around the head and neck, so have a close look at their scalp as well as neck.
- Don’t forget to check your pets, as well as outdoor clothing and other gear, for lurking ticks.

How do I remove a latched-on tick?
If a tick is removed within the first number of hours, the risk of it passing on an infection it might be carrying is very low. Just how long a tick takes to get settled before it starts feeding is not clear – it could be an hour or two, or several more.
Flicking off a tick may leave behind the head and mouth parts, from which the bacteria can continue to ooze into you, McKeown explains. Instead the entire tick should be removed with a tweezers by gripping it close to the skin, to try to avoid the mouth parts breaking off. It is a good idea to have a specially designed tick-remover, (available in pharmacies or shops that sell hiking equipment) on standby if the need arises – whether for use on a family member or on a pet.

Step-by-step instructions with images on how to remove a tick can be read in the section on Lyme disease on hse.ie or on ticktalkireland.org, the website of a patient support group.
What should I do then?
The skin where the tick was found should be washed with soap and water and an antiseptic cream applied. The area should then be checked over the next few weeks for swelling or redness. If the site of the bite develops into a red, pimple-like swelling within a day or two, it is probably nothing more than minor skin irritation but keep an eye on it.
What should I look out for after that?
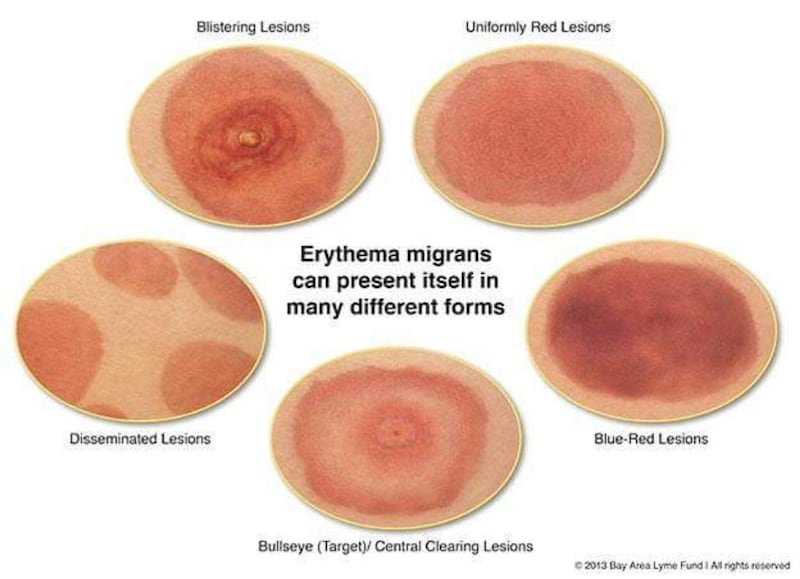
A clinically definitive sign of early Lyme disease is erythema migrans, commonly known as a “bullseye” rash due to looking like the centre of a dartboard. These are concentric rings of inflammation – red in the middle, surrounded by a pale circle, and then another red circle – and can appear anywhere on the body between a week and four weeks after a bite. If your child develops this rash, or any other sort of rash after you suspect they have been bitten by a tick, take them straight to a GP.
One sight of a bullseye rash should be enough for a GP to prescribe treatment with appropriate antibiotics over the next three weeks “and that will clobber it in 99 per cent of cases”, says McKeown.
That sounds straight forward enough…
Maybe for those with a bullseye rash that is caught early, yes, but in up to half of Lyme disease cases there will be no rash. Within four weeks of a tick bite, other signs that medical attention is required would include flu-like symptoms such as headache, joint pains and muscle aches.
There can also be neurological effects. One sign of the more severe form of Lyme disease, neuroborreliosis, is facial palsy – a droop on one side, as if they have had a stroke, says McKeown. “Very distressing whenever it happens but completely temporary.” Linking the many possible symptoms of chronic Lyme disease, which are similar to those of other conditions such as chronic fatigue syndrome and arthritis, to a tick bite can be problematic – particularly if you are unaware that there has been a tick bite in the first place.
How many cases of Lyme disease are diagnosed here each year?
That is not known because only the severe form, neuroborreliosis, is a notifiable disease that has to be reported to the Health Protection Surveillance Centre (HPSC) by doctors and laboratories. Approximately 10-20 cases of neuroborreliosis are recorded each year. Early cases of Lyme disease are not counted, McKeown explains, because that is a clinical diagnosis, usually on the basis of a bullseye rash. “People may be treated, and it might not be Lyme disease at all, it might be something else.” Whereas neuroborreliosis is diagnosed after a blood test.
The likely proportion of early Lyme disease cases to the incidence of neuroborreliosis is actively debated in international literature, he says. The HPSC estimates that there are up to 400 new cases of the milder form of the disease here annually. Dr John Lambert, infectious diseases consultant at the Mater hospital in Dublin, writing in the Irish Medical Journal, said modelling estimates would put that figure closer to 2,500.
All this is making me think twice about taking the children out for woodland walks . . .
Rest assured that when the very low likelihood of developing Lyme disease through a tick bite is weighed against the physical and psychological benefits of activities out in nature, the latter wins by a country mile. However, if you are more aware and follow the preventive advice above, you will be further reducing the risk.














